Mpox. What is it, where did it come from and how can the world deal with the threat?
Let us begin with what it is. Mpox, formerly known as monkeypox, is a viral disease that can spread between people, mainly through close contact, and from the environment to people via objects and surfaces that have been touched by a person with mpox.
According to WHO, MPOX originated from the DRC in 1970, and was neglected there. Prevalent in Central and West Africa, the infectious disease later caused a global outbreak in 2022, leading to a WHO public health emergency in July as it became a multi-country outbreak, Kenya being one of the affected countries, alongside, Rwanda, Uganda, and Burundi.
In Kenya, Mpox was declared an outbreak on July 31st, 2024, after a case was confirmed in Taveta Sub-County, Taita Taveta County. Kisii, Migori and Kiambu Counties also recently reported that they were investigating suspected cases of the disease. To combat the spread of this infectious disease, surveillance teams have been monitoring border points and transit routes. At the moment, testing is only being done at the National Public Health Laboratory, the Kenya Medical Research Institute (KEMRI) and CDC laboratories.
Mpox symptoms
Mpox manifests itself as a rash lasting for two to four weeks, which may be started with or followed by fever, headache, muscle aches, back pain, low energy and swollen lymph nodes. The rash looks like blisters and can affect the face, palms of the hands, soles of the feet, groin, genital and anal regions, mouth, throat or the eyes. The number of sores can range from one to several thousand.
The disease in infectious, and people who have it are considered infectious until all their blisters have crusted over, the scabs have fallen off and a new layer of skin has formed underneath, and all lesions on the eyes and in the body have healed. Typically, the duration for complete healing takes two to four weeks. It is important to note that people can be re-infected after they have had Mpox.

In most cases, the symptoms of Mpox go away on their own within a few weeks with supportive care, such as medication for pain or fever. However, in some people, the illness can be severe or lead to complications and eventual death.
Is it fatal?
People with severe Mpox may require hospitalization, supportive care, and antiviral medicines to reduce the severity of lesions and shorten the time to recovery. For a small minority. Between 0.1% and 10% of people who have become infected with Mpox, have died. Death rates in different settings may differ due to several factors such as access to health care and underlying issues including undiagnosed and advanced HIV.
Newborn babies, children, people who are pregnant, and people with underlying immune deficiencies such as from advanced HIV may be at higher risk of more serious Mpox disease and death.

Treatments and medication
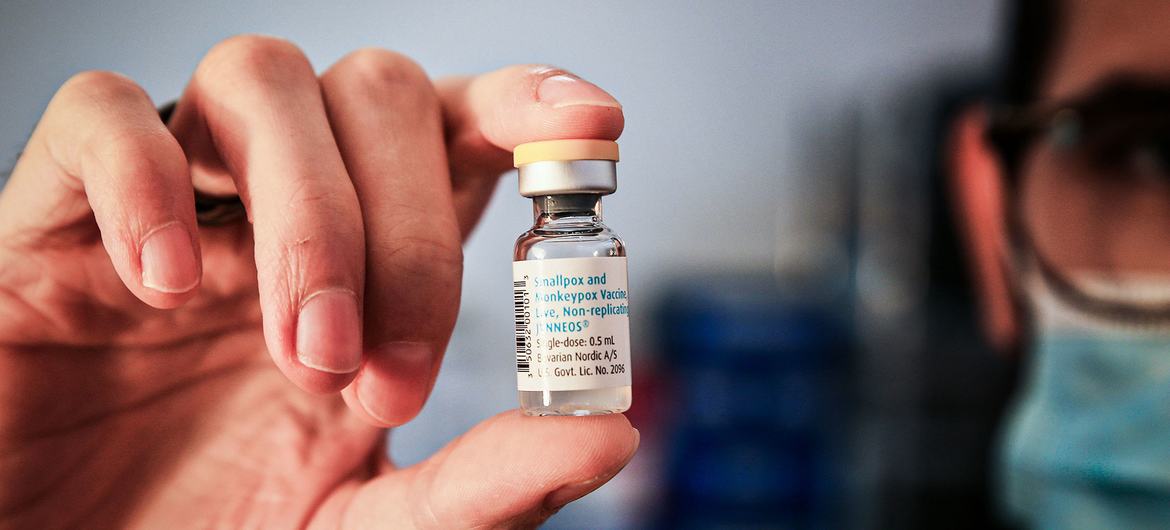
Thankfully, there is a vaccine to curb Mpox. WHO recommends several vaccines for use against Mpox, including the use of MVA-BN or LC16 vaccines, or the ACAM2000 vaccine.
In Africa, however, only Nigeria and the Democratic Republic of Congo have approved the vaccines. Kenya is yet to approve any Mpox vaccine for emergency use. According to the Ministry of Health, the country is currently concentrating on surveillance and testing suspected cases.
How to prevent Mpox
Like other infectious diseases, Mpox is preventable. Cleaning and disinfecting surfaces or objects and cleaning your hands after touching surfaces or objects that may be contaminated can help prevent transmission.
The risk of getting Mpox from animals can be reduced by avoiding unprotected contact with wild animals, especially those that are sick or dead.


